#CAIDEapp #dementiarisk #lateonsetalzheimersdisease
I've often stressed in my posts here over many years now that early risk assessments for Alzheimer's disease and vascular dementia is a prudent and vital strategy.
Is 24 years of age too early to begin tracking your risk for Alzheimer's and vascular dementia?
Consider this ... we've know for well over a decade that late-onset Alzheimer's disease (LOAD) has a traceable trajectory of at least 20 to 30 years to more.
Additionally, biomarkers that are linked to an increased risk for LOAD and vascular dementia are well established risk factors.
I first came across and understanding of the linkages for cardiovascular disease (CVD) and LOAD in the late 90s, and at that time wondered why medical professionals and Alzheimer's organizations were not actively alerting and advising the public about that association.
For example, the ApoE4 genetic risk variant is a significant risk factor for CVD AND LOAD, and you can control whether or not it becomes a factor in for CVD or LOAD as you age.
Ditto for all the other risk factors associated with ApoE4 such as type 2 diabetes, cholesterol imbalances, diet and lifestyle patterns, and the chronic inflammation and oxidative stress associated with it all.
A host of very accessible metabolic, biochemical, and genetic risk factors are very accessible and can shed a great deal of light on your risk for CVD, type 2 diabetes and LOAD throughout life.
Plus, the Cardiovascular Risk Factors, Aging, and Incidence of Dementia (CAIDE) score has long been used as risk assessment for CVD, LOAD, and dementia.
10 years ago, it was proclaimed that "The CAIDE Risk Score App is the first evidence-based App to estimate future dementia risk in midlife".
And now, in a study that included the CAIDE risk score in a study "which tracked a nationally representative cohort of adolescents since 1994-1995 ... the CAIDE score and cognitive function in young adulthood and early midlife in the U.S., showed that significant associations with cardiovascular risk factors can be observed well before age 50,”
For a more comprehensive overview of the role of type 2 diabetes and CVD in the risk for LOAD, please read "The Diabetic Brain in Alzheimer's Disease" which you can pick up on Amazon.
Think Ahead!
BrainDefend®
... See MoreSee Less
#dementiaawareness #EmergencyAssistance
Imagine having to rush one of your parents to an emergency room due to a psychotic or other type of urgent care need. So stressful.
Worse is the possibility that you may be stuck there for hours on end until someone can attend to your parents's care.
Or worse, having to leave them there as it may take days or weeks before there is an appropriate evaluation and followup—a nightmare scenario.
An emergency room visit is likely the last place you want to find yourself with a loved one who has dementia and is in need of immediate assistance.
As the report linked to here indicates, hospitals and their emergency care units are ill-equiped for the quick onboarding of a person with severe cognitive impairment.
As the incidence of Alzheimer's disease and other dementia-related causes continues to escalate here in the U.S. and around the world, families who are not aware of how to anticipate and plan ahead for the care of a family member that progresses from a seemingly harmless forgetfulness into a more severe cognitive impairment and eventual diagnosis of dementia will find themselves in a frantic rush to figure out what to do next.
The latter is particularly true for families who simply do not have the financial resources to seek professional guidance and care that can respond appropriately and expeditiously.
Instead, you may find yourself rushing to an emergency room for help—the last place you may want to find yourself in such a crisis.
Think ahead ... if a family member is experiencing any difficulties in executing their daily activities due to cognitive dysfunction, get to a medical professional ASAP for an evaluation.
Early assessment and interventions can make all the difference in the world, and keep in mind that a proactive approach and a personalized preventive plan may arrest a cognitive decline and prevent dementia.
Don't Wait To Be Diagnosed!
BrainDefend®
... See MoreSee Less
#tauprotein #alzheimerstest #biomarkers
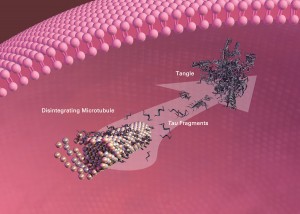
Over the last few years, I've posted here on the development of tau and beta-amyloid protein blood-based biomarkers in the assessment for Alzheimer's disease.
For example, in November-2020, I posted here that the much anticipated announcement for the first beta-amyloid blood test (Aβ42/40 ratio) for clinical use was finally here.
Similarly, blood test reports for plasma tau protein (phospho-Tau217) have shown significant promise for adjunctive assessment options to the Aβ42/40 ratio assessment.
Recent studies funded by the National Institute on Aging have shown that the blood samples of phospho-Tau217 (p-tau181) can serve as a viable biomarker for the early detection for early-onset AD many years before the onset of symptoms.
One such study concluded that "Blood measurements of ptau217 were also about 90% accurate at distinguishing people who later developed symptoms of dementia."
Plus, p-tau217 blood levels were deemed to be good as PET imaging and cerebrospinal testing for the specific development of AD.
And in 2023 (9/2023), I reported on the blood test—PrecivityAD2™—that includes a set of significant tau protein blood biomarkers—phosphorylated and nonphosphorylated forms of the p-tau217 and p-tau181 proteins.
Note that PrecivityAD2™is available to physicians from C₂N Diagnostics.
The backstory on the C₂N Diagnostics menu of tests is that the technology that underlies their p-tau217 assessment was developed by researchers at Washington University School of Medicine in St. Louis (WashU).
Now, and their most recent announcement, WashU researchers have developed another tau blood biomarker—MTBR-tau243.
The WashU report linked to here includes their rationale on the importance of another complimentary tau protein aggregate assessment (MTBR-tau243) that provides invaluable insights into the progression of Alzheimer's disease, and also is specific to Alzheimer's dementia.
The MTBR-tau243 evaluation viability was based on data extracted and validated from two cohorts that included individuals in the:
- presymptomatic stage of Alzheimer's disease (no cognitive impairment),
-through early-stage disease with mild cognitive impairments, and
- individuals with late symptomatic disease when patients exhibit full-blown dementia.
"The researchers’ analysis showed that blood MTBR-tau243 levels reflected the amount of tau tangles in the brain with 92% accuracy", and were independent of beta-amyloid aggregates.
Note well well (not included in the report) that neuroimaging tests such as PET, MRI and SPECT are accepted as valuable adjunctive tools for a biomarker guided approach for early diagnosis and treatment.
More importantly, while the tau and beta-amyloid tests are indeed important in the assessment of Alzheimer's disease stages—early to late stage—the most opportune timing in the evaluation of risk for late-onset Alzheimer's disease (LOAD) is midlife or earlier, and before any noticeable cognitive impairment is noticeable.
In combination with genetic profiling, cardiometabolic risk assessments, evaluations for hormone imbalances and deficiencies, and cognitive performance tests and others, such evaluations can also shed light on person's risk and vulnerability for LOAD as they age.
Don't wait to be diagnosed.
BrainDefend®
... See MoreSee Less
#metabolicsyndrome #type3diabtes #alzheimersrisk
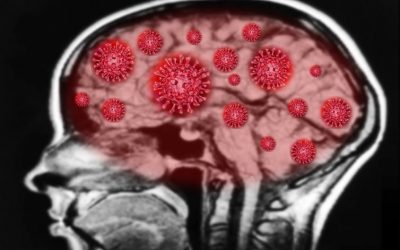
The incidence of age-related diseases such as type 2 diabetes/metabolic syndrome, and heart disease (cardiometabolic disease) and the risk factors associated with them, namely obesity, continues to escalate in a pandemic-like manner around the world.
Indeed, type 2 diabetes/metabolic syndrome, hypertension, obesity and cardiovascular disease (cardiometabolic disease), and the diet and lifestyle factors associated with them, vastly increases the risk for vascular dementia and AD, but they also MODIFIABLE risk factors. (The Diabetic Brain in Alzheimer's Disease).
The report linked to here highlights key genetic, and metabolic risk factor linkages which are strongly linked to the incidence of dementia and late-onset Alzheimer's disease (LOAD) including:
- ApoE4 gene variant
- disrupted fat metabolism (e.g., cholesterol/triglyceride metabolism)
- insulin function (e.g., insulin resistance)
- beta-amyloid aggregations (e.g., plaque)
- neuroinflammation (brain inflammation)
- brain shrinkage (atrophy)
The body and brain metabolic alterations linked to glucose and fat metabolism, insulin function derangements, and the the subsequent pro-inflammatory cascades driven by metabolic disease are again, modifiable risk factors and are reversible.
Dietary intervention therapies including ketogenic and caloric restriction therapies—the latter is not mentioned in the report—have an excellent track record of modifying the disease trajectories associated with metabolic disease and chronic inflammation.
Low-carb mediterranean diets are and excellent dietary management intervention as well.
Note: ketogenic diets are high fat diets.
Caution with the persistent caveat of "high-fat" dangers as it is often misinterpreted. Healthy fats derived from plant foods, and organic meat and dairy fats are a great source of nutrients.
Think ahead and take control of your risk; midlife is a critical juncture in the opportunity to do so.
More than one-third of the world-wide cases associated with the development of vascular dementia, and LOAD are linked to modifiable risk factors.
Seek the support of an experienced guide, and begin the process of understanding your risk for dementia and late-onset Alzheimer's disease through the assessment and evaluation of risk biomarkers, which can also shed invaluable insights for living younger, longer.
BrainDefend®
... See MoreSee Less